Menstrual migraines are headaches that show up around the time of your period. Many women call them hormone headaches because they are linked to monthly hormone changes. Unlike a usual headache, these headaches are strong, long-lasting, and can make daily life difficult. Doctors also use the term menstrual cycle headache or period headache.
Understanding why they happen, what they feel like, and how you can manage them can help you live with less pain. This article explains everything in simple language so you can finally get clear answers.
Table of Contents
ToggleOverview
What Is Menstrual Migraine (Period Headache)?
Menstrual migraine is a type of migraine linked to the menstrual cycle. These headaches happen two days before your period starts and up to three days after bleeding begins. They follow the same rules as other migraines but often last longer and feel more severe.
Doctors believe the main reason is the quick fall in estrogen that happens before bleeding starts. The hormonal change interacts with brain chemicals and blood vessels, leading to pain.
Many women notice that their strongest headaches always line up with their monthly cycle. This is why the term hormone headaches makes sense.
What’s The Relationship Between Hormones And Headaches?
Hormones like estrogen and progesterone play a key role in brain chemistry. Estrogen affects how brain cells communicate, how blood vessels behave, and how pain signals are controlled. When estrogen drops suddenly, the brain becomes more sensitive to triggers. This is why women get migraines more often than men.
Reproductive hormones and brain chemistry are deeply connected, and changes in these hormones explain why migraines often peak during menstruation, pregnancy, or menopause.
What Does A Hormone Headache Feel Like?
A hormone-driven headache is usually strong, pulsing, and focused on one side of the head. It worsens with movement. Light, sound, and smell can feel unbearable. You may also feel tired, dizzy, or nauseous.
How Common Are Menstrual Migraines?
Research shows that around 16 to 25 percent of women who get migraines notice a clear link to their cycle. Reports suggest that nearly 60 percent of women experience at least some cycle-related attacks. They are less common in men because male hormones do not go through the same monthly changes.
Symptoms And Causes
Menstrual Migraine Symptoms And Period Headache Signs

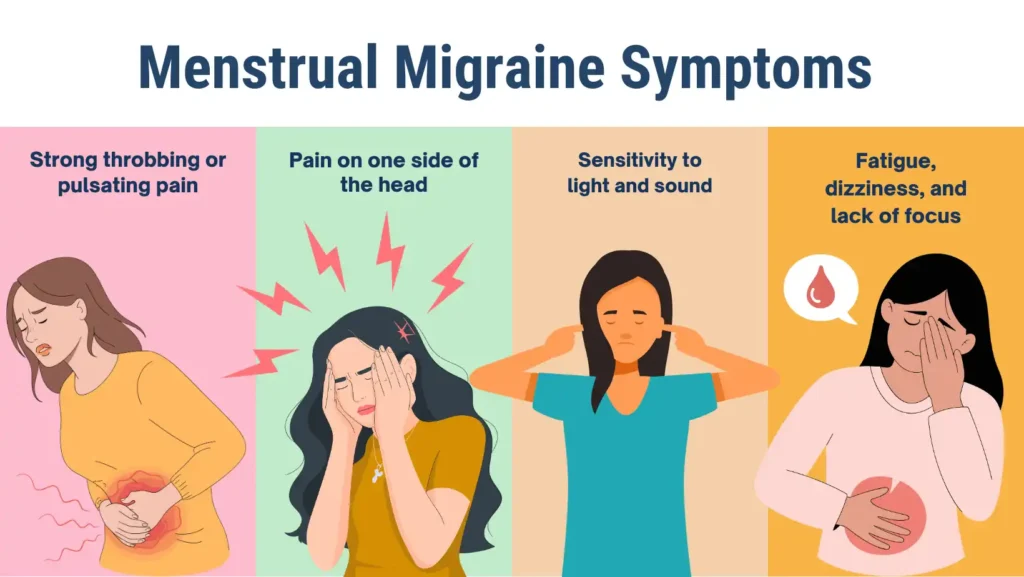
The most common menstrual migraine symptoms include:
- Strong throbbing or pulsating pain
- Pain on one side of the head, though it can move
- Sensitivity to light and sound
- Nausea or vomiting
- Fatigue, dizziness, and lack of focus
These attacks often last longer than non-menstrual migraines. A period headache may resist treatment and require stronger medication.
Where Are Menstrual Cycle Headaches Located?
Pain often begins behind one eye or on one side of the head. It can spread to the neck and shoulders. The exact spot can vary from month to month.
When Do Menstrual Migraines Start?
They usually start two days before bleeding begins and may continue for three days. Some women also notice an ovulation headache in the middle of the cycle when hormones shift again.
What Causes Menstrual Migraines?
You may ask, what causes menstrual migraines? The answer is simple: sudden hormone changes, especially falling estrogen, trigger these headaches. Other factors such as stress, poor sleep, or dehydration make them worse.
What Triggers Hormone Headaches During The Menstrual Cycle?
The main trigger is the estrogen drop and migraine link. As estrogen falls right before bleeding, brain sensitivity rises. Progesterone changes may also play a role.
Other hormone-related migraine triggers include:
- Skipping meals
- Excess caffeine or withdrawal
- Lack of sleep
- Stress
- Certain foods like aged cheese or processed meat
What Are The Risk Factors For Menstrual Migraines?
Women with a family history of migraines are more likely to get them. Those with heavy PMS symptoms may also notice headaches. Stress, birth control use, and irregular cycles increase the risk.
What Are The Complications Of Menstrual Migraines?
The main problem is quality of life. Pain can affect work, studies, and family life. Overusing pain medicine can cause rebound headaches. In some women, repeated attacks can develop into chronic menstrual migraines.
Diagnosis And Tests
How Is A Menstrual Migraine Diagnosed?
Doctors usually diagnose by history. They ask you to keep a headache diary, marking when the pain starts, how it feels, and when your period begins. If attacks line up with cycle days, the diagnosis is clear.
Lab tests or scans are rarely needed unless symptoms suddenly change, start later in life, or look unusual.
Do I Need To See A Specialist For Hormone Headaches?
You may not need a specialist if symptoms are mild. But if headaches are frequent, severe, or interfere with daily life, see a neurologist. They may suggest new treatments, especially if normal painkillers fail.
Management And Treatment
Menstrual Migraine Treatment Options
The best menstrual migraine treatment often combines early relief and prevention. Options include:
- Over-the-counter painkillers like ibuprofen or naproxen
- Triptans (sumatriptan, rizatriptan, zolmitriptan) taken at the start of pain
- Short-term preventive triptans or NSAIDs, started 2 days before bleeding
- Hormonal therapy, such as estrogen patches, for steady levels
- Daily preventive medicines if attacks are very frequent
Doctors sometimes use preventive migraine medication for women who suffer more than 4 attacks a month.
| Treatment Type | Examples | When Used |
| Pain relievers | Ibuprofen, Naproxen | At headache start |
| Triptans | Sumatriptan, Rizatriptan | Early attack |
| Hormonal options | Estrogen patch, birth control | Prevention |
| Preventive medicines | Beta-blockers, anti-seizure meds | Frequent cases |
Natural Remedies For Menstrual Migraines Without Medications

Many women prefer remedies for menstrual migraines that do not involve drugs. Common options include:
- Cold compress on forehead
- Rest in a dark, quiet room
- Steady meals to avoid sugar dips
- Drinking enough water
- Gentle yoga or relaxation
- Supplements like magnesium and riboflavin (with doctor advice)
Diet plays a role too. A balanced menstrual migraine diet rich in fruits, vegetables, and whole grains supports brain health. Limiting alcohol and processed food also reduces attacks.
Outlook / Prognosis
How Long Do Menstrual Migraines Last?
Each attack can last from 4 hours up to 72 hours. They often last longer than non-menstrual migraines. Treatment may be harder and slower to work.
What’s The Outlook For Menstrual Cycle Headaches?
The good news is that with proper care, most women reduce both frequency and severity. Some find relief after pregnancy or menopause. Others learn to manage triggers and use medication at the right time. While period pain and migraines can make life hard, a clear plan improves quality of life.
Prevention
Can Menstrual Migraines (Hormone Headaches) Be Prevented?
Yes, prevention works for many women. Doctors suggest short-term prevention with NSAIDs or triptans starting 2 days before bleeding and continuing for 3 to 5 days.
Hormonal strategies, such as birth control pills or estrogen patches, may help. Simple lifestyle changes for hormonal migraines also play a big role. Regular sleep, stress management, hydration, and balanced meals lower risk.
Tracking your cycle and noting triggers can help you stay prepared.
The Bottom Line
Menstrual migraines are not just “regular headaches.” They are linked to monthly hormone shifts and can be much harder to handle. Knowing what causes menstrual migraines and learning smart prevention strategies can reduce pain. Treatment options range from medicines to natural remedies.
Living with these headaches is tough, but with the right menstrual migraine treatment, life can become much easier. The key is tracking your cycle, planning ahead, and getting medical advice when needed.
FAQs
How do you treat menstrual migraines?
Treatment includes NSAIDs or triptans at the start of pain, short-term prevention around periods, and in some cases hormonal therapy or daily preventive medicines prescribed by doctors.
What does a menstrual migraine feel like?
It feels like a strong throbbing pain, often on one side, with nausea, dizziness, and sensitivity to light and sound. Movement usually makes the pain worse than usual headaches.
Why do I get migraines when I get my period?
Migraines often appear during periods due to sudden hormone changes. The quick estrogen drop just before bleeding triggers brain sensitivity, making the body prone to painful migraine attacks.
How long should menstrual migraines last?
They usually last between 4 and 72 hours. Menstrual migraines are often more stubborn than non-menstrual ones, making them harder to treat and more resistant to quick relief methods.
What to drink for menstrual migraine?
Water is the best choice. Small amounts of caffeine may help at the beginning of pain. Avoid alcohol. Magnesium-rich smoothies and herbal teas may also provide supportive comfort.
What are the 4 stages of a migraine?
The four stages are prodrome, aura, headache, and postdrome. Not everyone experiences all stages. Aura, such as visual changes, is less common but may appear in menstrual migraines.
What hormone deficiency causes migraines?
Migraines often come from a rapid estrogen drop, not simply low levels. This sudden change disrupts brain chemistry and blood flow, leading to sensitivity and migraine attacks during menstruation.
About The Author

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
Dr. Chandril Chugh is a U.S.-trained neurologist with over a decade of experience. Known for his compassionate care, he specializes in treating neurological conditions such as migraines, epilepsy, and Parkinson’s disease. Dr. Chugh is highly regarded for his patient-centered approach and dedication to providing personalized care.
→ Book a consultation to discover which remedies suit your needs best.