Foods and Drinks That May Help Manage Migraine
Foods to prevent migraines play a big role in how often attacks happen. The right meals give your…
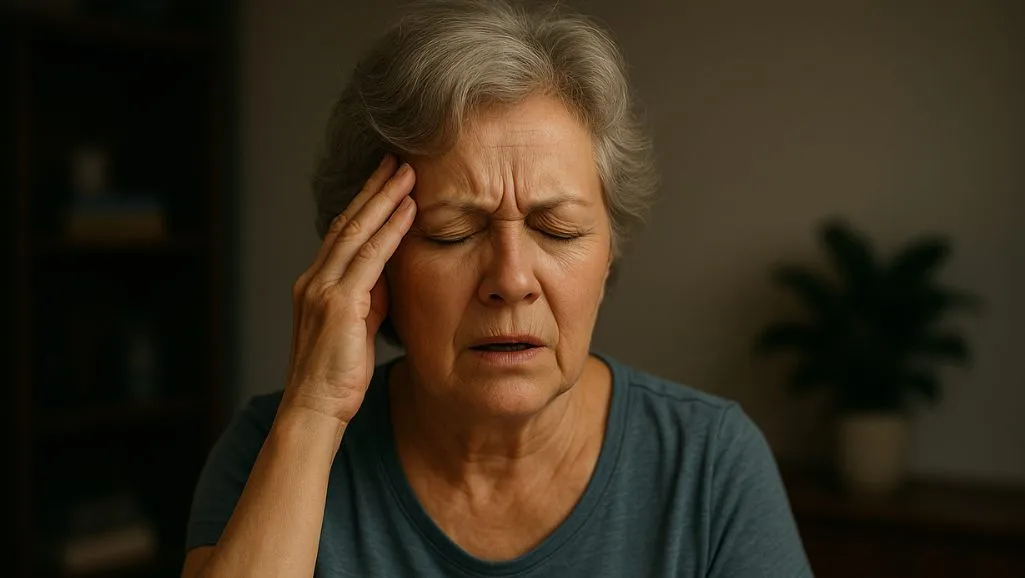
What causes migraine in females?
Migraines in females are more common in women than men, and the reasons go far beyond “just…
What Is Vestibular migraine?
Vestibular migraine is one of the most confusing migraine conditions. It does not always bring a…
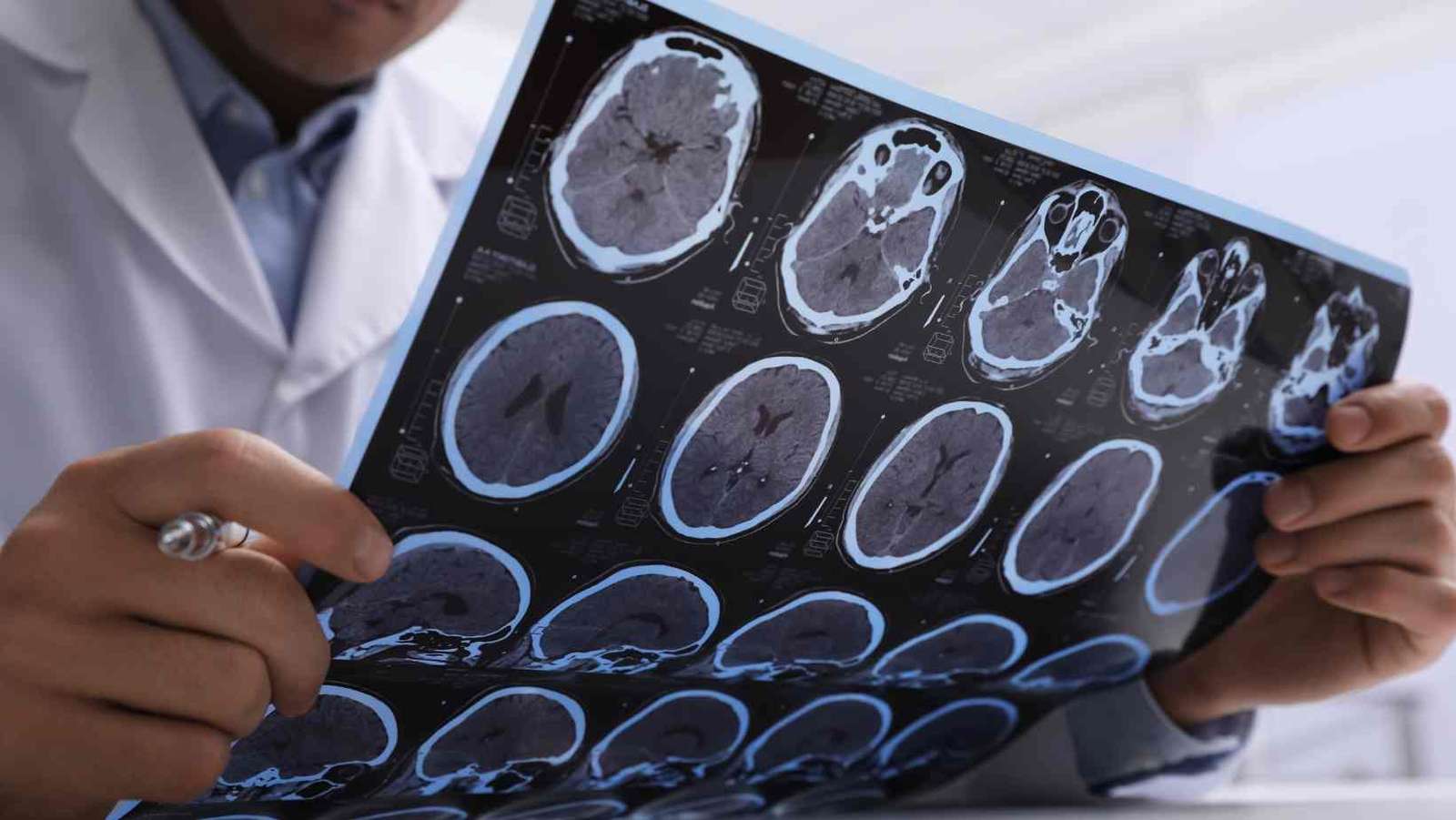
Concussion Symptoms and Treatment: What You Need to Know
A concussion is one of the most common brain injuries worldwide, yet it’s often misunderstood or…
What Is Encephalitis? A Complete Guide to Brain Inflammation
Encephalitis refers to a serious medical condition characterized by swelling of the brain. When…
Head Injury: Causes, Symptoms, and Treatments Explained
A head injury is more than merely a bump or bruise. It can affect the brain, skull, and scalp,…
What is Brain Surgery? Understand its Procedures, Benefits & Recovery Time
What is brain surgery? Brain surgery is a medical procedure where a neurosurgeon operates on the…
Understanding Brain Herniation
Brain herniation is one of the deadliest conditions in medicine. It happens when part of the brain…
Brain Disorders: Causes, Types, Risks, and Outlook
What are brain disorders? A brain disorder refers to any condition that negatively impacts the…
Acute Disseminated Encephalomyelitis (ADEM)
Overview What is acute disseminated encephalomyelitis (ADEM)? Acute disseminated encephalomyelitis…
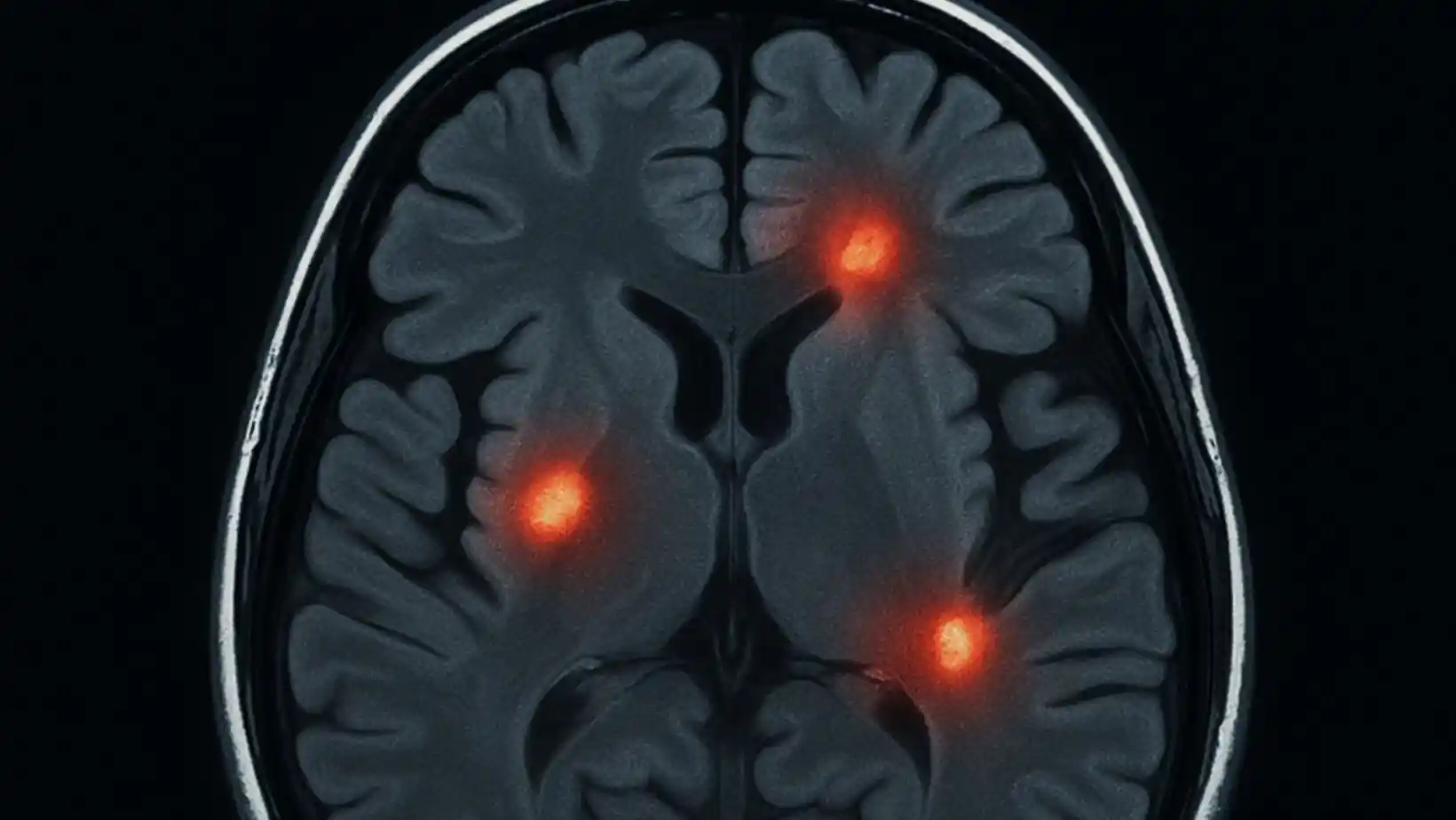
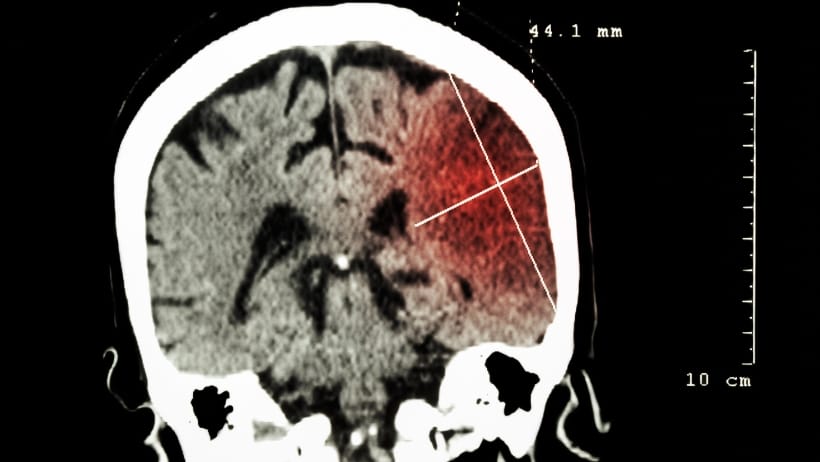
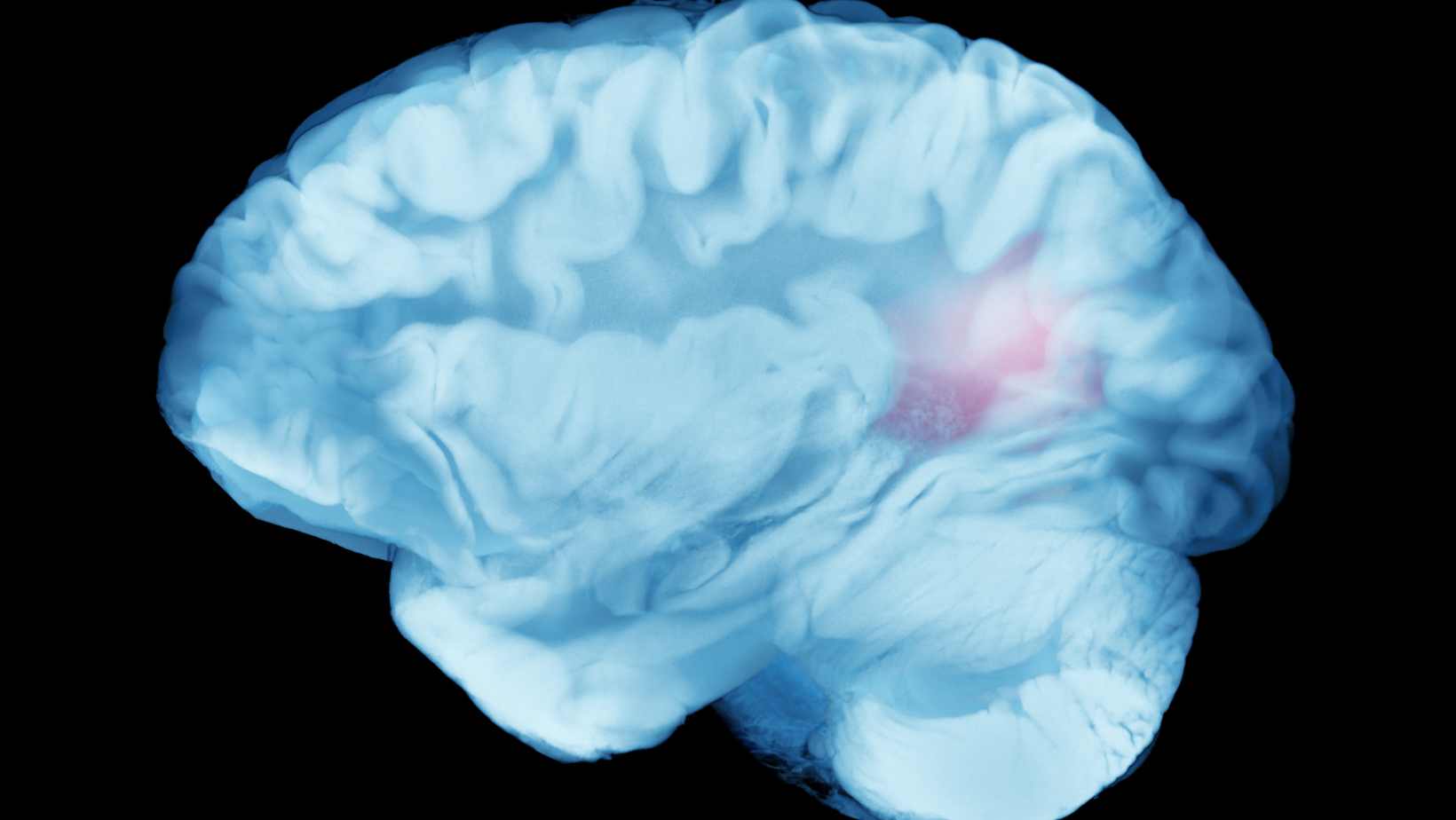
Migraine and Brain Lesions
What Are Brain Lesions? A brain lesion is an area where brain tissue is damaged. The damage can…
Brain Lesions: Causes, Symptoms, Treatments
Brain lesions are areas of damage in the brain tissue, and understanding them is crucial for your…
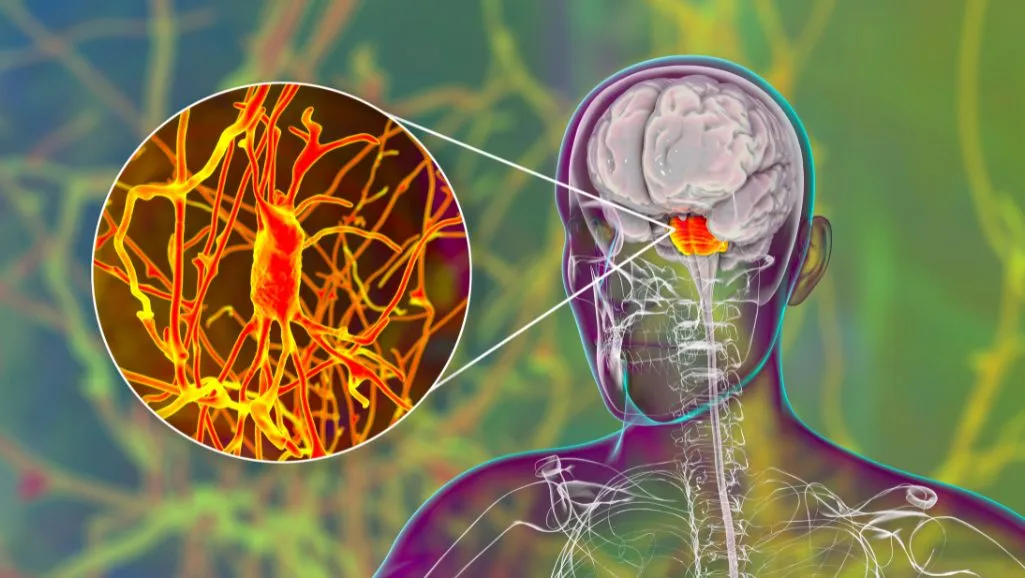
Neuroinflammation Demystified: Triggers, Symptoms, and Treatments
Neuroinflammation is the brain’s defense mechanism. When it detects a threat, like toxins,…
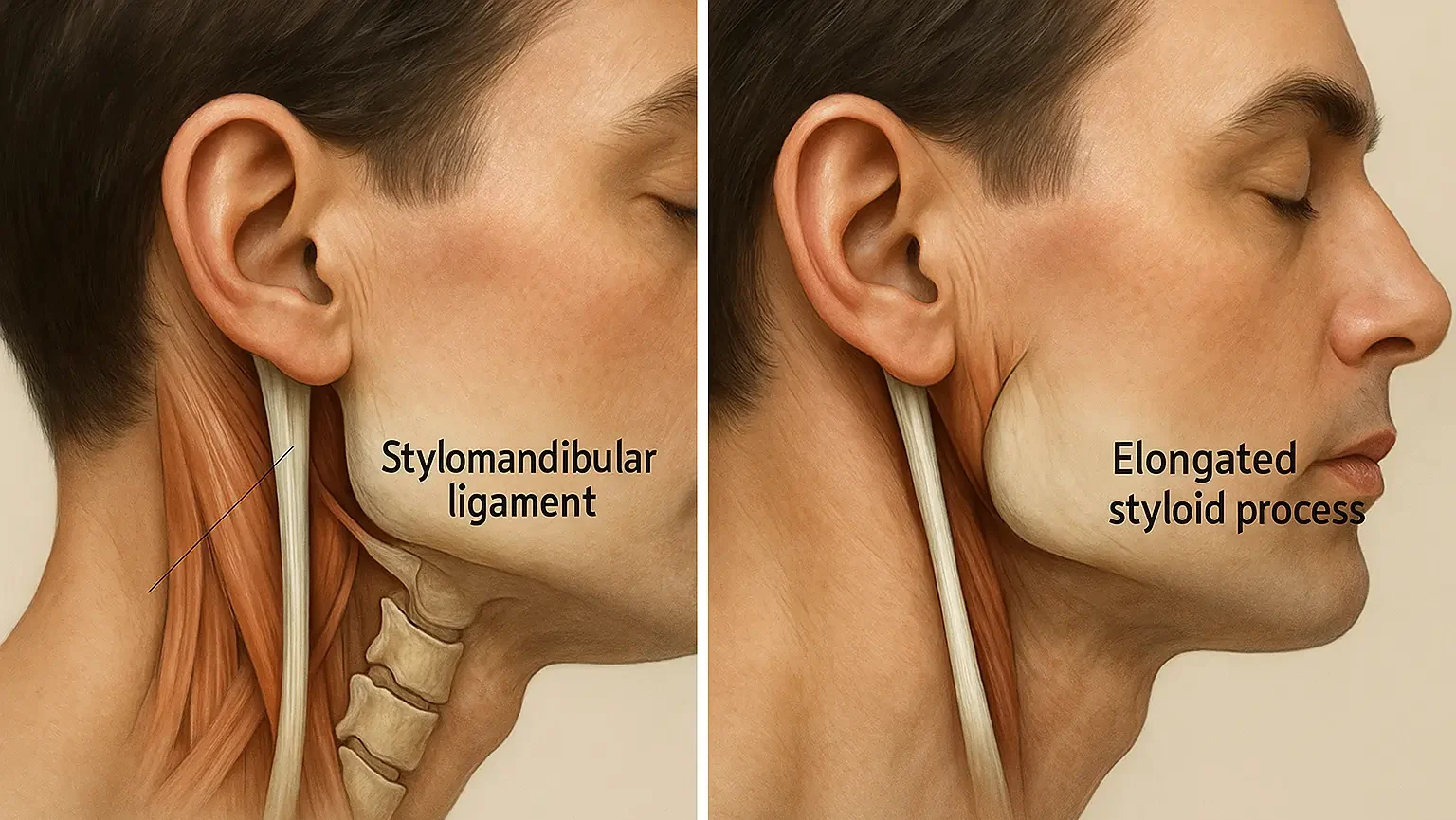
Ernest Syndrome vs. Eagle Syndrome: Differences, Symptoms, Causes, and Treatments
Eagle syndrome and Ernest Syndrome are two rare but painful conditions that affect the head and…
Posterior Reversible Encephalopathy Syndrome (PRES)
Posterior Reversible Encephalopathy Syndrome (PRES) is a brain condition that causes sudden…
What is Uncoordinated Movement?
Uncoordinated movement is when the body struggles to control motion properly. It can affect…
Transient Ischemic Attack (TIA)
Transient Ischemic Attack is a short-term blockage of blood flow to the brain. Though symptoms may…
What is Friedreich’s Ataxia? Understanding the Basics
Friedreich’s ataxia is a rare, inherited condition that quietly alters how the body works. It…
Acute Cerebellar Ataxia (ACA)
Acute cerebellar ataxia doesn’t give you a warning. One day you may walk normally. The next day,…
What Is Cerebellar Ataxia? Understanding the Basics
Cerebellar ataxia refers to a condition in which your brain has difficulty managing balance,…
Neurologist-Backed Natural Remedies for Improving Nerve Strength
If you have ever felt tingling, numbness, or pain in your hands or feet, it’s a sign that your…
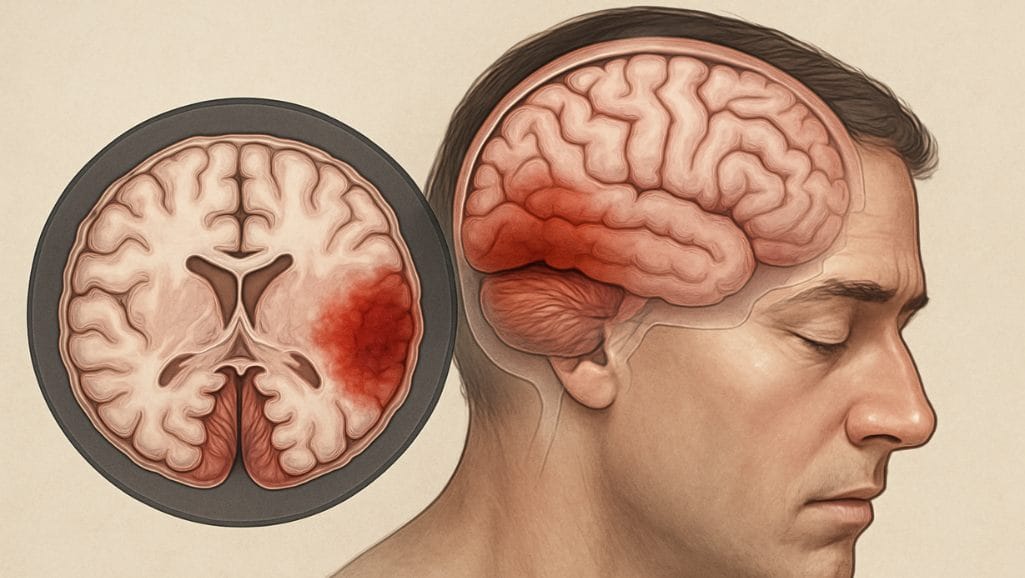
Treatment of Brain Hemorrhage: Causes, Symptoms & Options
A brain hemorrhage can be a frightening term — and rightly so. When bleeding occurs in or around…
Superfoods for Brain: Boost Memory & Cognitive Health Naturally
Did you know nearly 60% of your brain is made of fat, and what you eat directly impacts your…
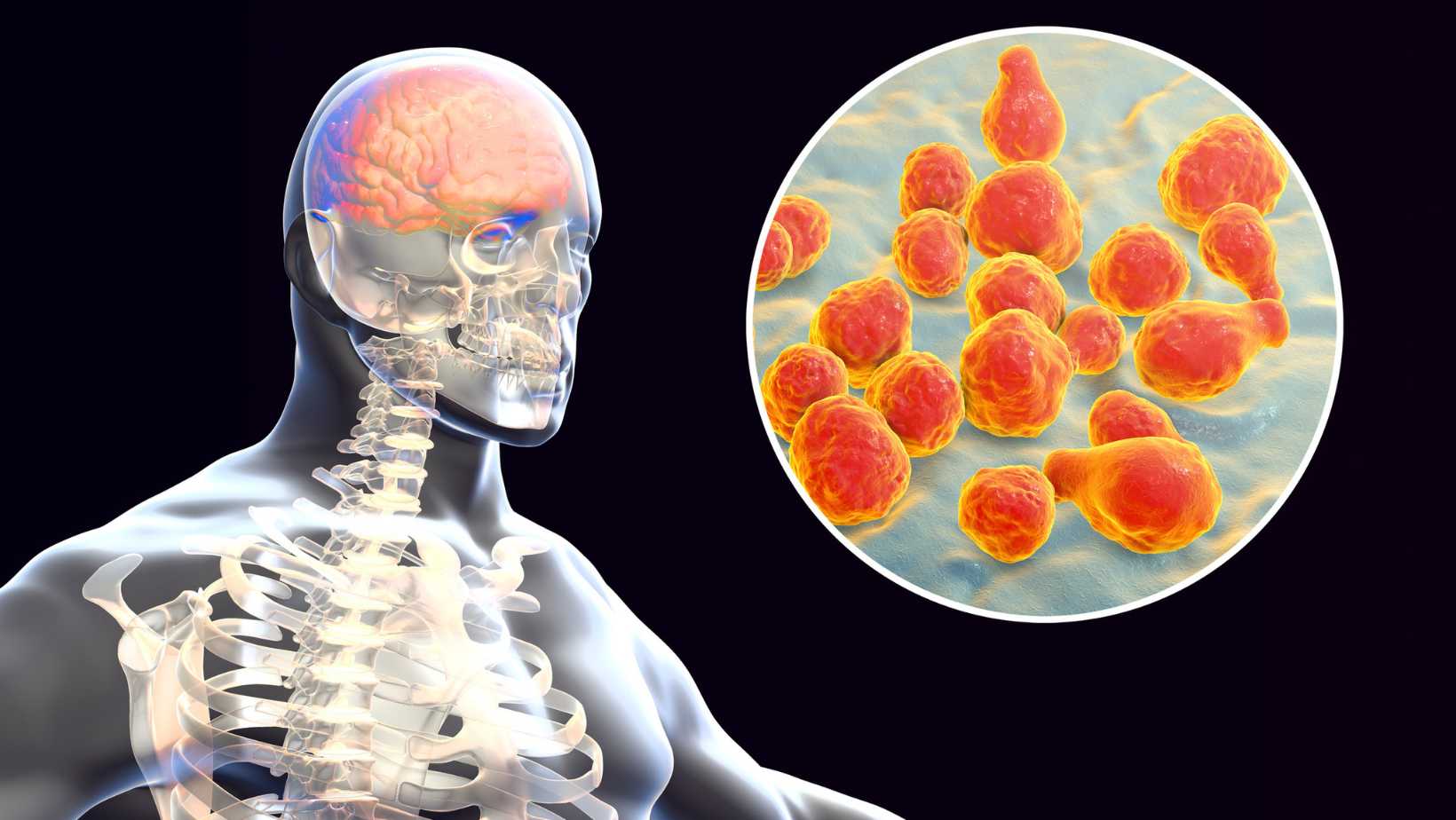
What is Neurosyphilis? Causes, Symptoms & Diagnosis Guide
Have you ever heard about syphilis affecting the brain? That condition is called neurosyphilis, and…
Arnold Chiari Malformation Radiology Insights
Arnold Chiari Malformation (CM) is a condition where brain tissue extends into the spinal canal,…
Masters in Child Psychology: A Complete Career Guide for Future Mental Health Professionals
Did you know that 1 in every 7 children between the ages of 15 and 24 suffers from mental health…
How to Build a Daily Routine for Optimal Mental Performance
What if your brain wasn’t tired because of overwork but because of poor routine? Most people think…
How to Stay Motivated in the Summer
Summer is a season that naturally invites a slower pace. The long days, warm weather, and…
Can Meditation Improve Sleep for Those With Anxiety?
Sleep problems are common among people with anxiety. Racing thoughts, tension, and stress can make…
Vitamins for Postpartum Depression: Do They Help?
Hey there, amazing new mama! You've just accomplished something incredible, bringing a whole new…
Understanding Pseudotumor Cerebri Symptoms: What to Look For
Pseudotumor cerebri is a condition where pressure inside your skull rises without any clear cause.…
Treatment for Essential Tremor: What Works Best?
Essential tremor is a common neurological condition that causes uncontrollable shaking—usually in…
Amyotrophic Lateral Sclerosis Diagnosis: How It’s Done and What to Expect
Amyotrophic Lateral Sclerosis (ALS) is a progressive neurological disorder that affects the motor…
Effective Ways to Reduce Stress in Your Daily Life
Feeling overwhelmed lately? Daily stress can sneak in through work, home, or even the endless…
Effective Basilar Artery Migraine Treatments
Have you ever experienced a strange kind of headache that comes with blurry vision, dizziness, or…
Therapy for Separation Anxiety: What Works Best?
Ever feel that knot of worry tightening in your stomach when a loved one walks out the door? Or…
Exercise for Back Pain: Effective Routines for Relief and Prevention
Back pain is one of the most common reasons people miss work or visit a doctor. But here’s the good…
Effective Brown-Séquard Treatment Options
Ever felt like your body's playing a bizarre trick on you, where one side feels weak while the…
Effective Facial Palsy Treatment Options
Hey there! Ever felt like one side of your face decided to take an unexpected vacation? Maybe a…
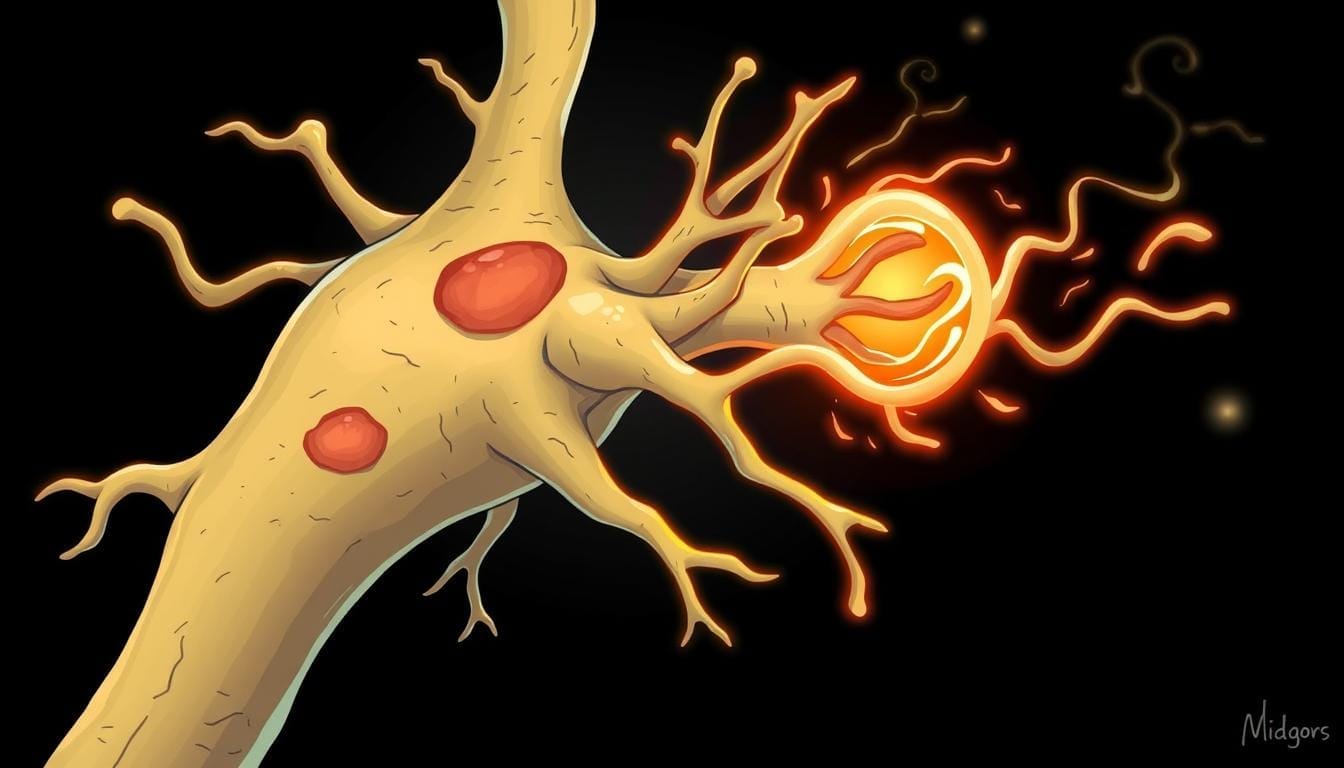
Nerve Growth Factor: The Key to Healing Damaged Nerves?
Imagine your body has a secret repair crew, tiny workers constantly striving to mend and rebuild…
The Impact of Smartphone Use on Sleep Patterns
We check our phones before bed, scroll endlessly through social media, and sleep with them under…
How Stress Affects Brain Development in Children
Most parents notice when their child is upset or anxious. But very few realize how deeply it can…
13 Major Day-to-Day Things You Do That Can Damage Your Brain
Ever wonder why some kids seem to bounce back from tough times while others struggle? The answer…
How to Prevent Nerve Damage Through Diet and Exercise
Tingling fingers? Persistent numbness in your toes? That electric shock feeling that just won't…
Can Stress Cause Brain Tumors? Revealing the Truth Behind the Myth
Ever feel like life's constant pressures – the never-ending to-do lists, looming deadlines, and…
Can Stress Cause Neurological Disorders? What You Need to Know
Ever wondered why you forget things more often when you’re stressed out? Or why your head starts…
Brain Aneurysms Uncovered: 24 Critical Questions Answered by a Neurologist
As a neurologist, I've stood alongside countless individuals and their families confronting the…
How to Manage Everyday Life with a Neurological Condition
Living with a neurological condition doesn’t mean giving up on your daily life. Yes, the symptoms…
Is Your Diet Cola Making You Dumb?
Artificial sweeteners are everywhere hidden in diet sodas, sugar-free snacks, “health” drinks, and…
Hereditary Spastic Paraplegia Physical Therapy: How Movement Can Reclaim Life
Hereditary spastic paraplegia (HSP) can make even simple movements feel like a battle. With legs…
Is Sex A Common Cause Of Brain Stroke?
Sex and stroke—two words that rarely appear in the same sentence, yet for some, they intersect in…
Understanding Machado Joseph Disease: Symptoms and Management
Some conditions quietly take root, unfolding their effects over years before a diagnosis is even…
Causes of Mononeuritis Multiplex: Understanding the Underlying Factors
Mononeuritis multiplex is a neurological condition that can affect a person’s quality of life in…
Dandy Walker Syndrome Treatment Options
"Why is my child developing slower than others? Why are their movements not like other kids?"…
Relationship Between Caffeine and Sleep Quality
Caffeine is part of daily life for millions of people across the globe. From the comforting aroma…
Surgical Management of Meningitis: When is Surgery Needed?
Introduction: Understanding Meningitis and Its Treatment Meningitis is a serious infection that…
The Truth About ADHD Medication in India – Expert Advice by Dr. Chugh
Imagine your mind as a symphony, but the instruments are playing out of tune. That’s ADHD.…
Nerve Pain Relief: Strategies for a Better Quality of Life
Unleash Yourself from the Grip of Nerve Pain: Discover 10 Transformative Strategies for a Life…
Mind-Body Techniques for Nerve Healing: Stress Reduction & More
Ever feel like your nerves are frayed, buzzing with phantom pain or tingling sensations long after…
Foot Neuropathy and Diabetes: Special Considerations
Imagine your feet as your body's roots, grounding you in the world. Now, picture those roots slowly…
Natural Remedies for Neuropathy: Healing Nerve Pain Without Medication
Say Goodbye to Neuropathy: Natural Treatments That Work Tingling toes? Burning feet? Is that…
Nerve Pain Relief: Beyond the Pills
Nerve pain can be a relentless, disruptive force, impacting every aspect of your life. It's often…
Nerve Damage Doesn't Have to Be Forever: Exploring the Possibilities of Repair
Imagine waking up every morning with numb fingers, a burning sensation in your feet, or a sharp,…
Is It Possible to Reverse Neuropathy Fast? What a Neurologist Says
Tired of simply coping with the relentless tingling, numbness, and pain of neuropathy? It’s…
How I Cured My Neuropathy: A Personal Journey to Nerve Pain Relief
Tingling feet? Numb fingers? That constant burning sensation that just won’t quit? If you’re…
10 Tips for Supporting Nervous System Development in Children
Childhood brain development is a key time for growth and potential. Parents and caregivers can help…
How to Manage Sleep Disorders in Neurological Patients
Sleep disorders are common in people with neurological conditions. They affect up to 30% of this…
The Connection Between Sleep Deprivation and Cognitive Decline
Have you ever had a night where you barely slept and couldn’t focus the next day? Maybe your memory…
Why Sleep Quality Matters More Than Sleep Quantity
Sleep is key for our survival. For years, we've focused on how much we sleep. But now, we see how…
The Role of Play in Cognitive Development
Play is key in building trust and is full of empowering and connecting moments. It helps overcome…
Debunking the 8 Hour Sleep Rule: What You Need to Know
Do you really need 8 hours of sleep every night? Many believe this is a strict rule for good…
How to Create a Bedtime Routine for Adults That Promotes Brain Health
A consistent bedtime routine is key for good brain health and overall well-being. The U.S. Centers…
The Role of Storytelling in Child Development Psychology
Storytelling is a key tool in child development psychology. It helps grow young minds in many ways.…
Early Signs of Developmental Delays in Children
Developmental delays are a big worry. About 1 in 6 kids in the U.S. face at least one delay. These…
The Link Between Diet and Childhood Cognitive Growth
Is your child's food helping their brain grow or slowing it down? Parents across the world want…
How Music Therapy Benefits Children With Autism
Music therapy is a powerful way to help children with autism spectrum disorder (ASD). It uses music…
How Childhood Trauma Impacts Adult Mental Health
Childhood adversity, or ACEs, has a big impact that lasts a long time. Studies link ACEs to mental…
Foods to Avoid If You Have Neurological Disorders
Neurological disorders can greatly affect a person's health and happiness. Diet is key in managing…
The Connection Between Nerve Damage and Chronic Pain
Why does your pain never seem to go away, even after the injury heals? What if your own nerves Have…
The Importance of Neurological Health Checkups
Keeping the nervous system healthy is key for overall wellness. Regular checkups are vital for…
Understanding the Role of Neuroplasticity in Recovery
Have you ever wondered how some people start walking again after a stroke or trauma, even when…
The Impact of Hydration on Neurological Health
What if the cause of your brain fog isn't stress or overwork but something as simple as not…
How to Use Nutrition to Support Nerve Regeneration
Peripheral nerve injuries hit over one million people worldwide each year. They cause big problems…
How Energy Drinks Affect Cognitive Performance
Energy drinks have become very popular since the late 1990s. They claim to boost physical…
How to Spot the Early Symptoms of Neurological Disorders
Neurological disorders can affect many areas, like thinking and moving. They touch millions of…
The Role of Genetics in Neurological Diseases
Genetics has changed how we see neurological diseases. These conditions can come from one bad gene…
Supplements to Boost Brain Function
Have you ever found yourself forgetting names, losing focus mid-sentence, or struggling to stay…
The Impact of Caffeine on Memory and Focus
Have you ever grabbed a cup of coffee before a big exam or an important meeting, hoping it will…
Ways Parents Can Support Emotional Health in Children
Have you ever wondered why your child seems more withdrawn, easily upset, or just "not themselves"…
Best Snacks for Studying and Staying Focused
Ever caught yourself yawning mid-revision or forgetting everything you just read? You're not alone.…
5 Yoga Poses for Better Sleep and Relaxation
Have you ever spent hours staring at the ceiling, trying to fall asleep but your mind just won't…
Top Methods for Herniated Disc Pain Relief: Effective Solutions
If you're one of the 2% of adults in the U.S. with a herniated disc, you know the pain is real and…
Men's Health and Mental Health: Why It Matters
Your mental health is as vital as your physical health, especially for men. Dr. Chandril Chugh, a…
Depression in Men: Symptoms and How to Seek Help | Dr. Chandril Chugh
Depression is a serious mental health issue that affects both men and women. But, depression in men…
Abnormal Child Psychology: Key Concepts and Insights
Abnormal child psychology is a key area in psychology. It looks into behaviors in kids and teens…
Disturbed Mental Health in Older Adults
As the world's population ages, we face a big challenge with the mental health of older adults.…
Anxiety in Adolescence: Recognizing and Managing Symptoms
The teenage years are tough, and it's key to spot and tackle anxiety in our young ones. Anxiety is…
Top Characteristics of Mental Health: What You Need to Know
Do you ever wonder what makes someone truly mentally healthy? Is it being happy all the time? Is…
Guide to Adult Mental Health Services
Every year, about one in five American adults face mental health issues. Life events and changes…
Top Interventional Pain Management Techniques for Chronic Pain Relief
If you're dealing with chronic pain, you're not alone. Millions worldwide struggle with constant…